Ett kortare inlägg om hur immuniteten jämför sig efter infektion med SARS-CoV-2 (COVID-19), kontra efter vaccinering mot COVID-19. Vi har nu data som tyder på att Omicron sänker skyddet från vaccinen, och även vid tidigare COVID-19. Därav är det enligt många (t.ex. FHM, ECDC och CDC) viktigt att vaccinera med en 3:e vaccindos (hos fullvaccinerade), och åtminstone med 1 (men helst med 2) doser hos de med genomgången COVID-19. Anledningar redovisas i en längre utläggning nedan, liksom i min tidigare bloggpost här. Se även längre ner Folkhälsomyndighetens rekommendationer, som är de som gäller.
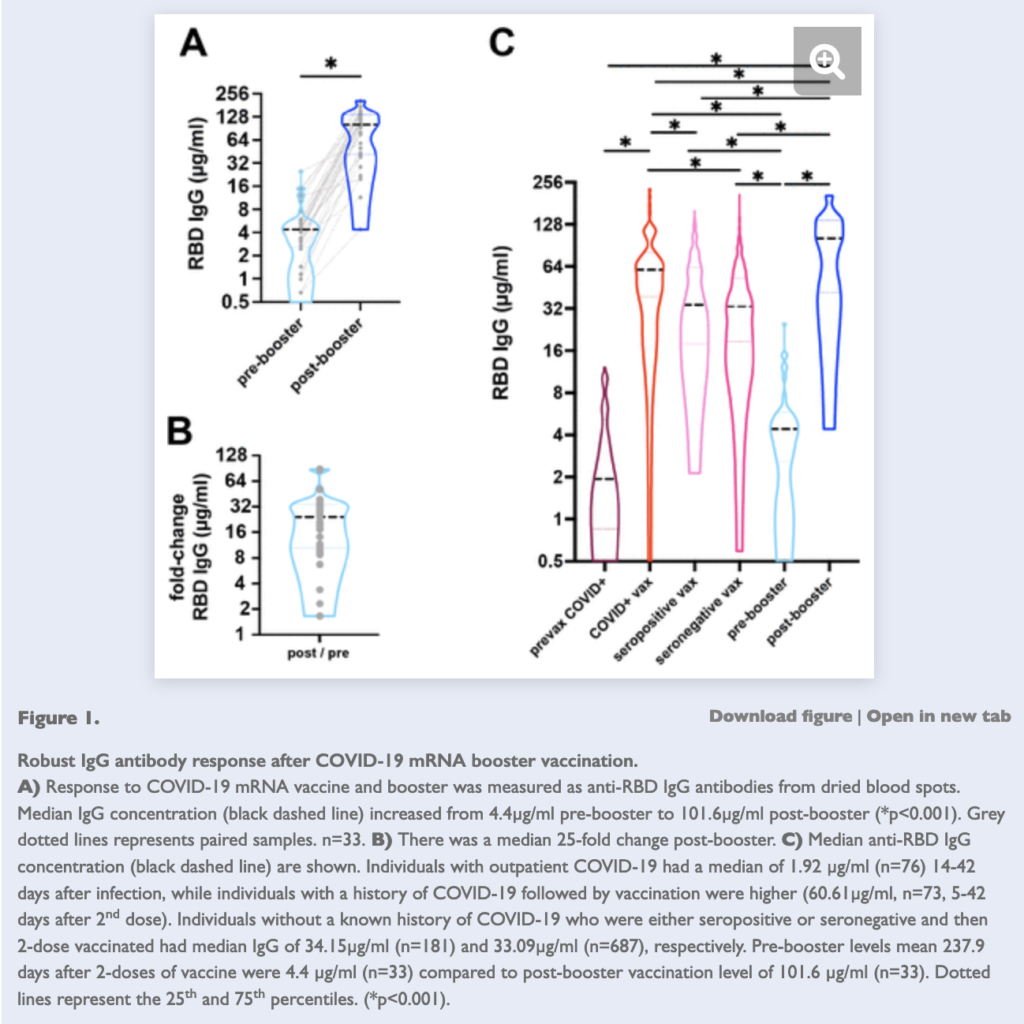
Dels finns det en variabilitet i immunsvaret efter genomgången infektion – en betydande andel serokonverterar inte enligt flera studier (se återigen mitt tidigare blogginlägg, samt denna tråd). Nivåerna av neutraliserande antikroppar är därtill mycket variabla över tid efter COVID-19. Antikroppsnivåerna (mot spike-proteinet som man vaccinerar mot) är därtill t.ex. över lång tid betydligt högre efter vaccinering jämfört med efter COVID-19, och 99% av alla som vaccineras serokonverterar (dvs. i princip alla med ett normalt fungerande immunförsvar).
Att antikroppsnivåerna åtminstone initialt är högre efter vaccinering, är ett fynd som ses genomgående i många studier, åtminstone för mRNA-vaccinen. Nivåerna tycks emellertid (av naturliga skäl) gå ner fortare från den initialt mycket höga nivån, efter vaccinering (se även mitt tidigare Facebook-inlägg här – den i inlägget beskrivna studien har nu publicerats i tidskriften Vaccines). Till detta kan man tillägga preliminär data som tyder på att de som har fått 3 vaccindoser, uppvisar högre antikroppsnivåer än de som bara har haft COVID-19 och hade vaccinerats med 2 doser, samt givetvis betydligt fler än de som bara hade haft COVID-19 (det kan givetvis finnas variation eller selektionsbias i denna studie; se även punkt 3 i mitt tidigare blogginlägg om Omicron här).
Samtidigt tycks just tre vaccindoser – utifrån antikroppsbaserad immunitet – också på många sätt överträffa eller vara likvärdigt med den som fås av tidigare COVID-19 och efterföljande vaccinering, eller genom genombrottsinfektion efter tidigare tvådosvaccinering (se tråd här).
De olika typerna av immunitet tycks därmed hålla olika väl över tid utifrån olika aspekter och analyser, och denna bild kan givetvis ändra sig ytterligare med tiden och nya varianter (många argumenterar vidare för att det vore konstigt om det inte i de flesta fall – men med ovan nämnda variabilitet – sågs en hyfsat god och lång immunitet mot svår COVID-19, efter en sådan genomgången infektion, eftersom man exponeras för så mycket av viruset, och så många olika virusproteiner).
Men exponering för virusets proteiner på ett av sätten – genom en SARS-CoV-2-infektion – är givetvis betydligt mer riskabelt.
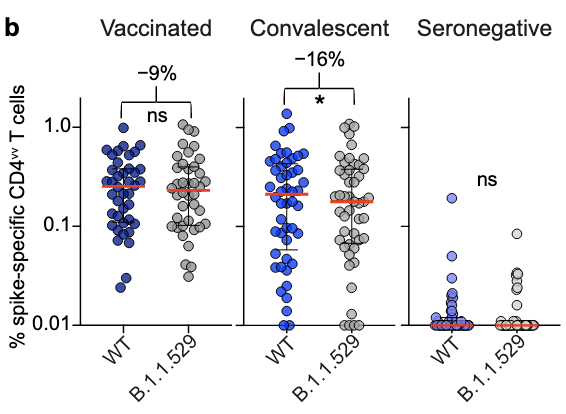
Om något tycks det immunologiska T-cellssvaret ur flera aspekter kunna vara något sämre mot Omicrons Spikeprotein, hos de med tidigare COVID-19, jämfört med efter vaccinering, enligt en ny studie i Nature Medicine av forskare från Karolinska Institutet. Detta fynd gäller både på CD4+ och CD8+ T-cellssidan. T.ex. sågs 8% lägre CD8+ T-cellssvar mot Omicrons Spike-protein hos de som hade vacccinerats med två doser Pfizers mRNA-vaccin (BNT162b2), medan reduktionen var 30% hos de som tidigare hade haft COVID-19 (maximal reduktion var 55% respektive 63%). För CD4+ T-cellssvaret var reduktion icke-signifikant på 9% hos de vaccinerade individerna, kontra signifikanta 16% hos de med tidigare COVID-19 (se skärmdumpen nedan, från Gao et al.).
När de slog samman CD4+ och CD8+ T-cellssvaret mot Omicron, sågs ett försämrat svar hos de som tidigare hade haft COVID-19, men ingen reduktion i svaret hos de som hade vaccinerats. Notera att de med tidigare COVID-19 i denna studie hade smittats under våren 2020, så de var inte smittade med de senare varianterna (såsom Alpha, Beta eller Delta). Resultaten kan därmed eventuellt skilja sig för de som smittats av andra varianter av SARS-CoV-2.
Annan data tyder på ett likvärdigt T-cellssvar mot Omicron hos de med tidigare COVID-19, jämfört med de som har vaccinerats. Givetvis får man dock efter vaccinering inte ett T-cellssvar mot lika många proteiner – vaccinen immuniserar mot Spike-proteinet.
Så man kan inte heller påstå att genomgången COVID-19 i sig skyddar bättre rakt av, det blir missvisande – även om många analyser finner att i snitt så har de med tidigare COVID-19 ett bra eller rentav bättre skydd i jämförelse med vaccinen över tid – åtminstone under Delta-perioden (se preprintsstudien av Gazit et al., samt ny publicerad CDC-data).
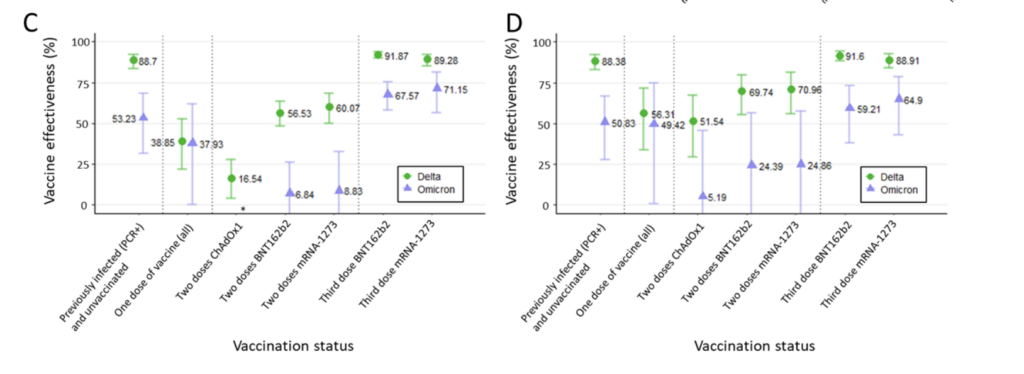
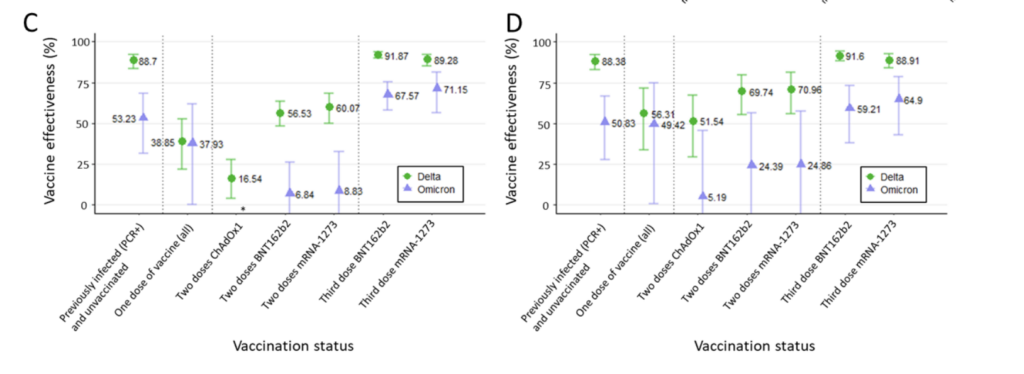
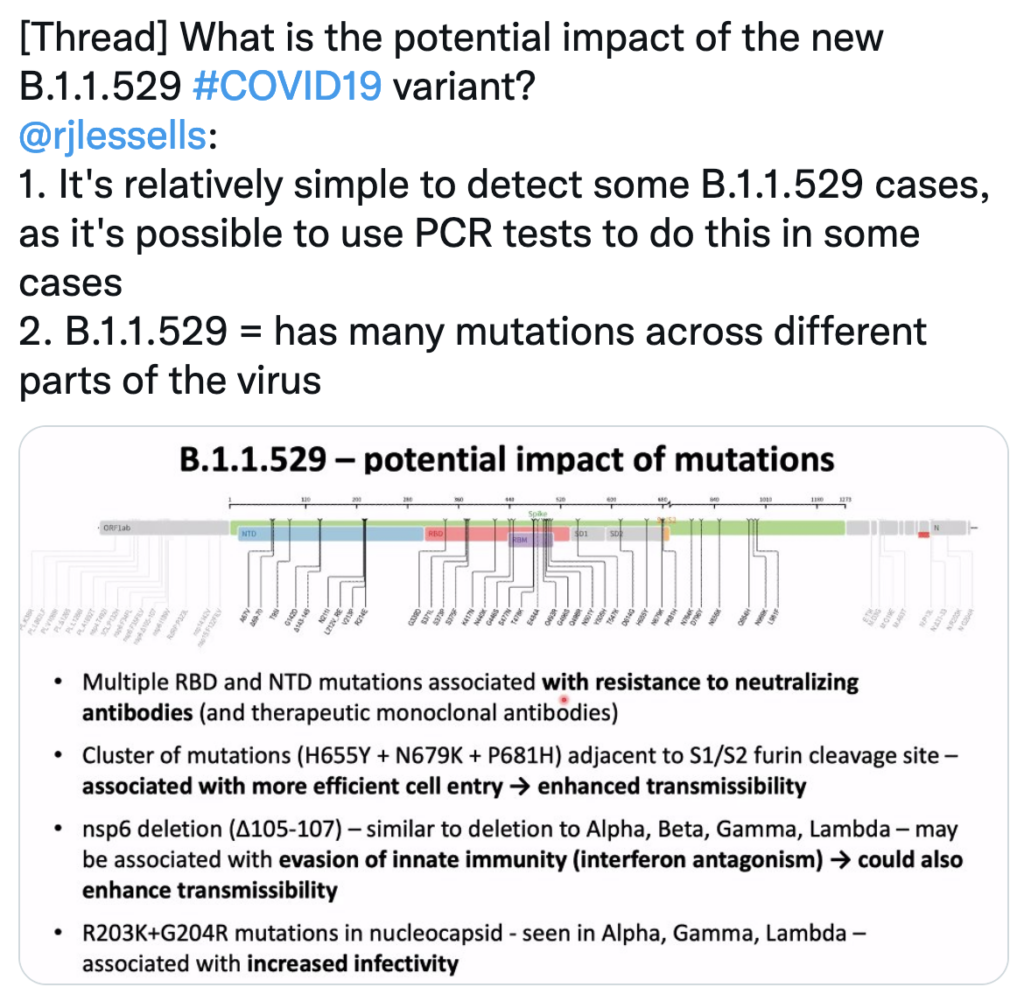
Detta skydd (både efter tidigare COVID-19 och medierat av vaccinen) har dock försämrats betydligt i och med Omicron, åtminstone vad avser skyddet mot infektion/symptomatisk COVID-19. Därutöver, om man tittar under den tidigare Alpha-perioden (visserligen närmare inpå när vaccinen hade getts och antikroppsnivåerna är så höga), så hade i stället de med COVID-19 sämre skydd mot infektion, än fullvaccinerade individer (och som teknikalitet är detta därtill ingen preprintstudie, utan redan publicerad i Nature Medicine). Denna fördel för vaccinen sågs även i den ovan nämnda CDC-artikeln.
Allt detta är då återigen med den brasklappen, att det innebär en mängd risker att smittas med SARS-CoV-2 och riskera olika former av COVID-19 och dess följdeffekter – inte minst död i sjukdomen (risker som i snitt är betydligt lägre vid en reinfektion, efter tidigare immunitet). Mer om det kan ni läsa i mitt tidigare blogginlägg här, samt i denna studie av Barda et al. i NEJM.
I stället anses vaccinen vara oerhört säkra, något som är redovisat i många analyser i peer-review-granskade tidskrifter från flera olika länder, och av varandra oberoende forskare, samt utifrån miljontals givna doser – även avseende riskerna för hjärtat (även om det finns en låg risk, liksom det finns med de flesta vaccin). Det finns därtill nu data för skyddet som fås av 2 och 3 doser vaccin, upp till 3-4 månader mot Omicron-varianten.
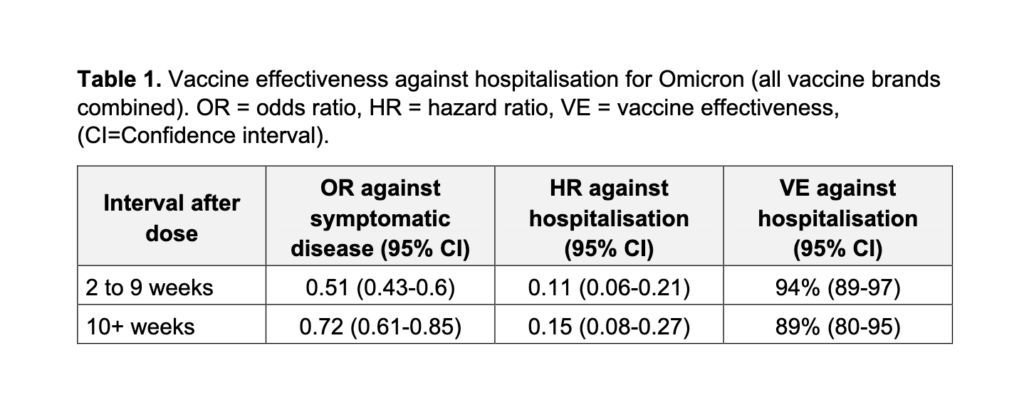
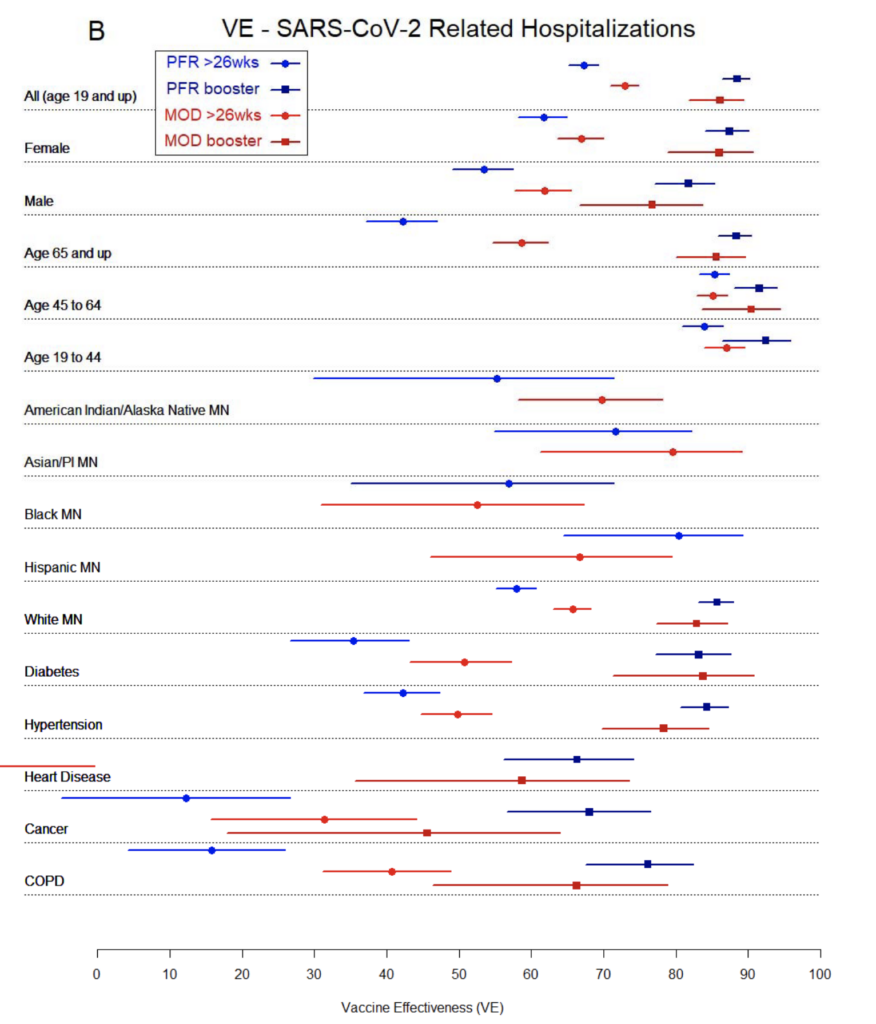
Att 3 doser kan ge ett gott skydd mot svår COVID-19, har observerats i analyser av stora delar av den allmänna befolkningen (ålder 18+) samt för äldre individer (65+), som utgör en riskgrupp för svårare COVID-19. Datan visar att överlag, med 3 vaccindoser, erhåller man i snitt runt 90% skydd mot svår COVID-19 orsakad av Omicron-varianten, och detta i åtminstone 3 månaders tid (se gärna här, samt mitt uppdaterade blogginlägg här). En full vaccinationsserie har samtidigt tidigare visat sig ge lägre risk för en reinfektion för de som tidigare har haft COVID-19.
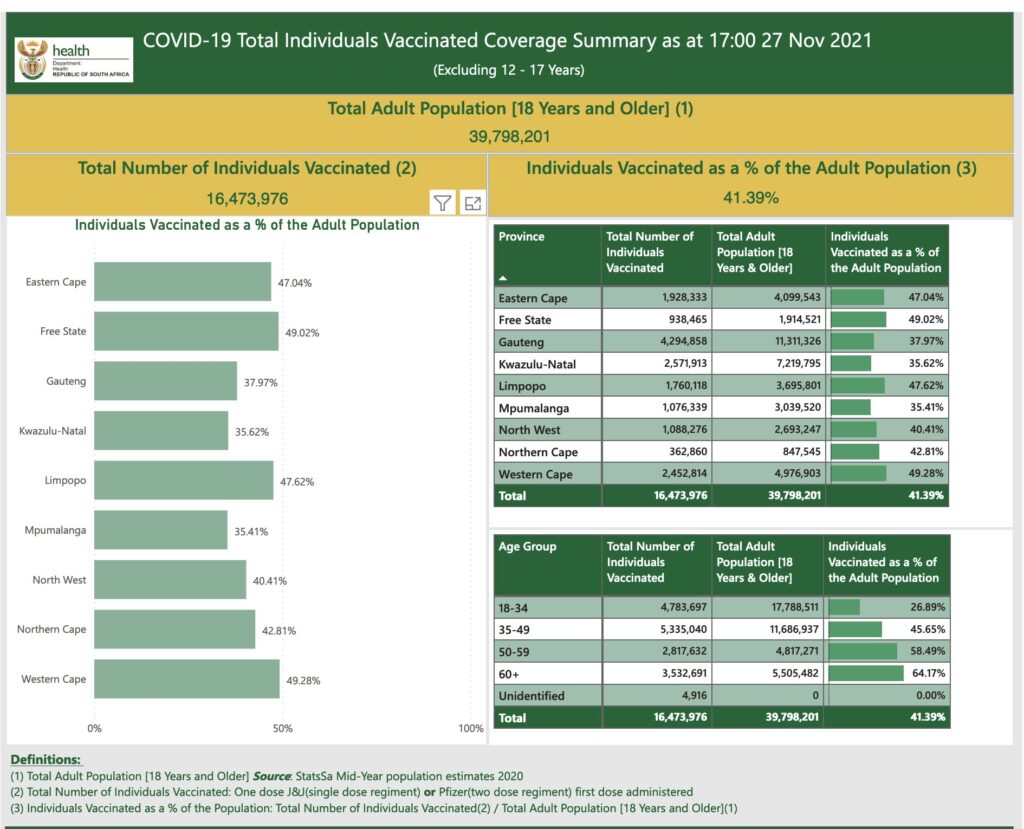
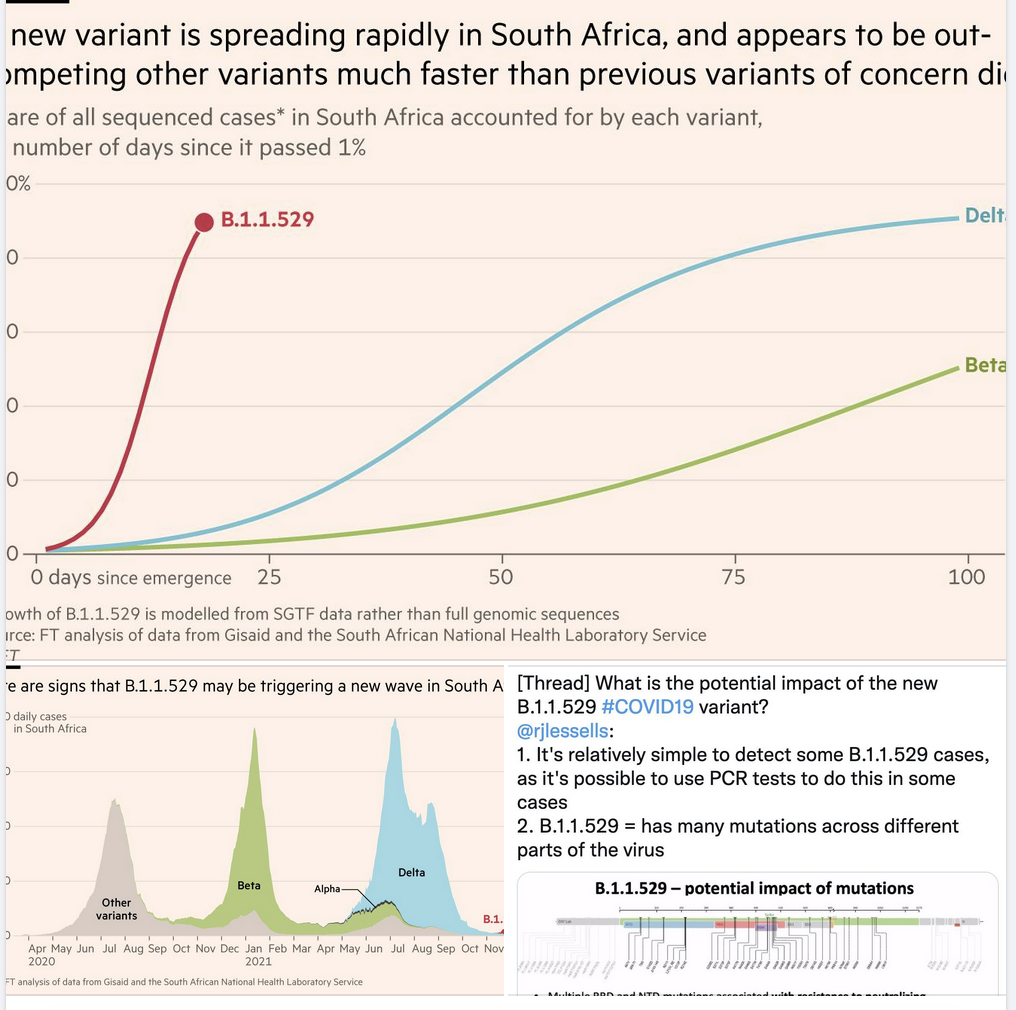
Antikropparna håller sig därtill enligt ny preliminär data på relativt hög nivå – mot just Omicron – upp till 4 månader efter den 3:e dosen. Men oavsett det är alltså risken för reinfektion (efter tidigare COVID-19) eller genombrottsinfektion (vid vaccinering) alltså betydligt förhöjd med den nu dominerande Omicron-varianten (B.1.1.529).
Därav har t.ex. ECDC tidigt under Omicrons spridning – liksom nu WHO, för vuxna – påpekat vikten av att vaccinera med en 3:e dos. Vid tidigare COVID-19 anser många experter att man åtminstone borde ta någon vaccindos (i det senare fallet anser en del att det är bättre med två vaccindoser, se även punkt 2 här i mitt tidigare blogginlägg). En del argumenterar därför för att man ska erkänna tidigare COVID-19 som att motsvara skyddseffekten av en vaccindos.
Här är det viktigt att påpeka att t.ex. Folkhälsomyndigheten och CDC alltså anger att man ska vaccinera sig även efter genomgången COVID-19. Liksom jag redovisar ovan nämner de som anledning att man inte vet hur varaktigt skyddet efter COVID-19 är, att skyddet efter COVID-19 är variabelt, samt att vaccinationen då [ytterligare] minskar risken att man smittar andra (Detta tycks även i viss mån gälla under Omicron-smittspridningen, i alla fall ifall om man tittar på de som har fått åtminstone två, men särskilt tre vaccindoser – noter att detta också är en preprintstudie som därmed behöver granskas externt). Folkhälsomyndigheten anger även att man ska ta en boosterdos (vid det angivna dosintervallet), även om man tidigare har haft COVID-19.
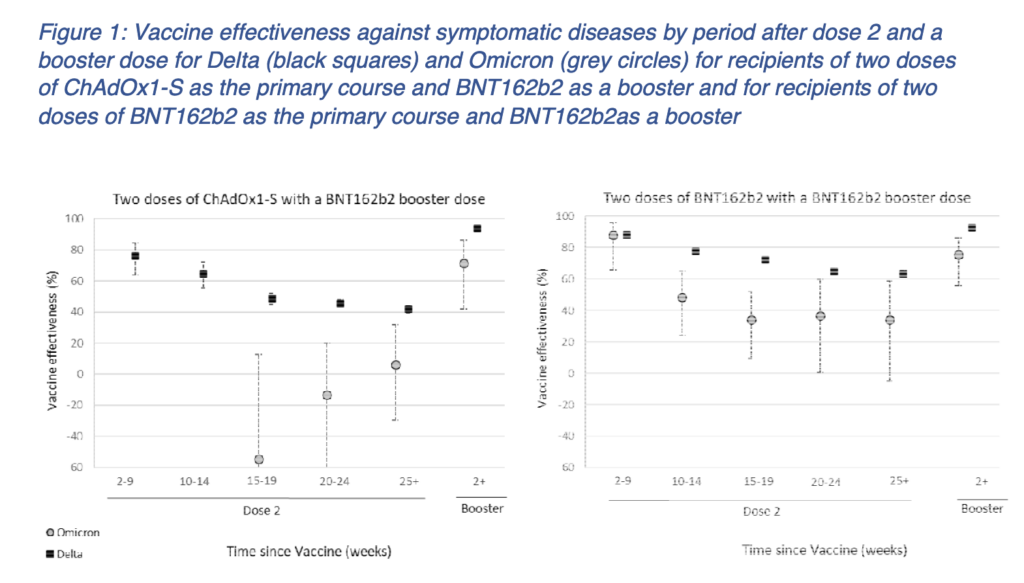
Sen är det även missvisande att som vissa gör påstå att vaccinskyddet alltid är mer kortvarigt och “begränsat”. T-cellssvaret efter vaccination består liksom efter COVID-19 också väl över tid, även vid en given dos som är lägre än de nuvarande använda vaccinen (25 µg här, kontra 30 µg i Pfizers, och 50-100 µg i Modernas vaccindoser, se Mateus et al., Science 2021). Ni får vidare gärna läsa punkt 3 i mitt tidigare blogginlägg, där jag går igenom hur vaccinskyddet har hållit väl över tid, inklusive under Deltaperioden, dvs. en period som inträffade flera månader efter många hade vaccinerats i t.ex. USA (som de flesta av studierna i inlägget berör).
Ovanstående berör bara ett urval av alla studier, och det kommer givetvis komma fler jämförelser över tid, t.ex. fler långtidsstudier avseende skyddseffekten av olika typer av tidigare immunitet mot Omicron-varianten.
Med vänliga hälsningar,
Jonathan Cedernaes
Leg. läkare, PhD, docent i medicinsk cellbiologi
Screenshot below from Figure 1b. Gao et al. Nature Medicine 2022, showing the T-cell response against WT and the Omicron variant (B.1.1.529) of SARS-CoV-2.